Introduction
The Treadmill Health and Care System describes a future based on ever-increasing need being put on the NHS and ever-decreasing funding being available. Staff are being expected to do ever-more with ever-less simply to stand still and maintain safe levels of service and care.
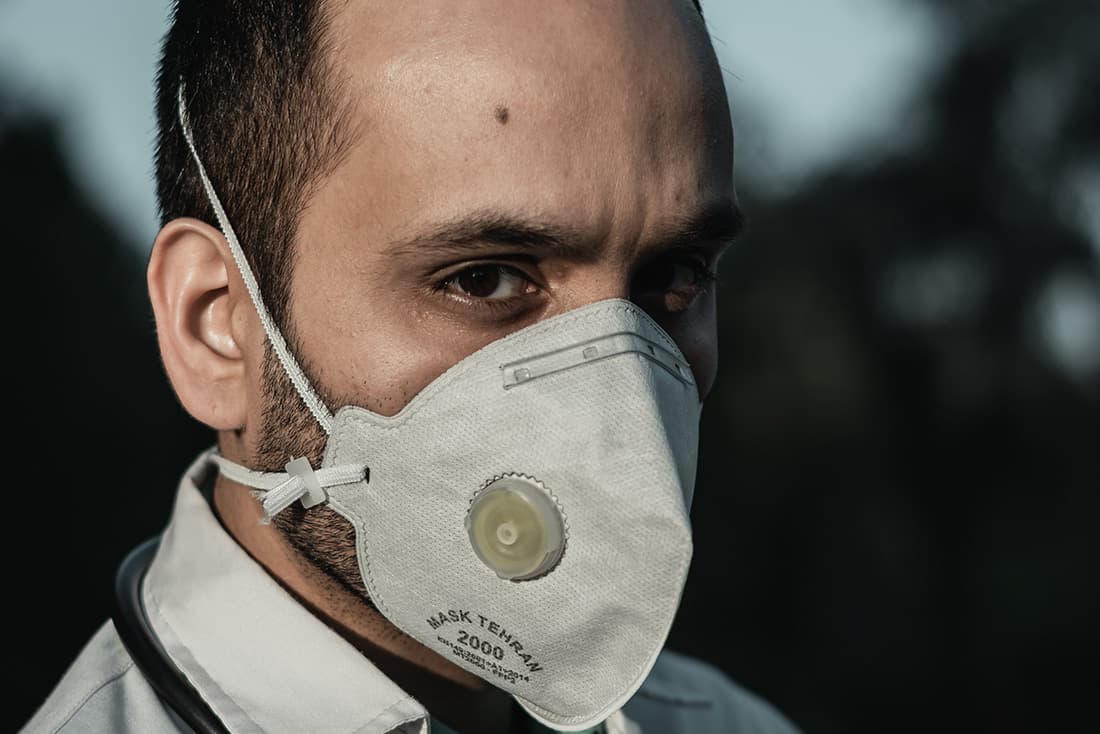
The public have allowed this to happen, and politicians have failed to act. Since the Covid pandemic of 2020/21 the public have demanded more investment into the NHS system to try to ensure provision, but the reality is that consecutive reforms have failed to address the underlying issues.
What will it be like in 2035?
- Years of increased demand and decreased relative funding will lead to the NHS being unable to offer acceptable standards of care to all.
- Integration of health and social care will fail to produce a responsive care system in the South West
- Those relying on the NHS will not be able to access many services locally and will be expected to travel or use slow and outdated technologies.
- The NHS workforce in the South West will be understaffed and many local services have closed in recent years.
- Significant demand for staff support will be needed to manage the MH pandemic of covid and post-covid unmet demand leading to 90% of NHS resources being spent on staff.

A view from 2035
Today in 2035, many commentators report that the NHS workforce feels betrayed. After the great Pandemic Public Inquiry of 2022, political promises were made to invest in the NHS which did not materialise. Instead, NHS services began to be dismantled because of funding shortfalls which have impacted significantly on staffing levels. There are few incentives to retain specialist consultants locally with the best being recruited to National Centres of excellence and Big Pharma. The export of clinical specialists to the US (the UK’s primary health partner post Brexit) has left the specialist workforce in the SW depleted and recruitment and retention are now regular critical agenda items for system leaders. There are few specialist centres and large hospitals in the South West anymore and people have to travel great distances for specialist care.
The promises of politicians and health chiefs to work closely with clinicians and other health professionals to identify ways to reduce duplication in how clinical services are delivered translated into deep cuts. Sweeping changes have been made to criteria for access to services in both physical and mental health services. Psychological services are reduced to acute admissions and containment therapies only with a return to 1950s style institutionalised care for large swathes of the South West population. Talking therapies have become the domain of private therapists and regulation of therapists is now voluntary following the unmanageable increase in individual therapists setting up as sole traders in the aftermath of the cuts to MH services. As a consequence, suicide rates are at an all-time high and the newly established suicide service set up in 2030 to cope with the demand from individuals and families affected by suicide is now overwhelmed. Mental distress is a ticking time bomb for UK society and as a predominantly rural community, the South West Suicide Service has lost track of wider community needs and become focused on Bristol and Plymouth communities only.
Musculoskeletal service demand is at an all-time peak and the cut off point for any diagnostic intervention is age 35. GPs are now required to refer over 35s to private sector consortiums of physiotherapists and osteopaths and many larger employers have developed in house deals with private sector providers as a way to mitigate impact on workforce capacity. Beyond large employers, those with private resources pay for their treatment whilst the majority of people with MSK conditions self-medicate with a range of painkillers and steroid treatments available from online pharmacies.
The largely successful economic growth targets for the South West region have been neutralised by the soaring cost of care across all sectors and a financial zero-sum game has been declared by the South West Regional Office for Government. Successive breakdowns in relationship between system leaders charged with aligning economic and health agendas has contributed to the fragmentation of health and economic factors in the South West. This has shown up significantly in the leadership of local Alcohol Plans.
Despite liver disease now being the third largest cause of death in the South West, the development of the 2034 Bristol City Alcohol Plan marked an all-time low in South West integration relationships. On 25 March 2034, the Bristol Economic Wellbeing Board met in Room 1 of Bristol House to approve a £93 million Waterfront Bars and Restaurant proposal whilst at the same time, in Room 2, the Health and Wellbeing Board were signing off a £96 million pound rescue package for a new Liver Unit at Bristol Hospital.
The irony was not lost on community campaigners and a petition was launched by members of the former 2023 Collaborative Communities Forum, demanding that the two Boards meet to align objectives for the City’s Alcohol Plan. The petition did not receive enough signatures to be considered by officials and despite local efforts to mediate between the two Boards, their refusal to meet resulted in two competing strategies for Alcohol in the City being signed off. For political reasons, this was not addressed by the Regional Council in 2034 and today, in 2035 there is confusion and fragmentation at all levels of implementing the Alcohol Plan in Bristol, including different approaches to licensing regulations approved by each Board. Local families and individuals affected by addiction bear the cost of this breakdown of leadership. The Bristol example is indicative of the breakdown of system leadership relationships across the South West region.
The long-awaited reform of social care following the increased awareness of the interdependencies between hospitals and nursing homes has led to an increasingly medicalised approach to care of the elderly. Care homes now fall under the remit of the Director of Nursing and every South West hospital now has a Care Dependency Unit (CDU) with limited bed numbers available at any one time for admission. Staff are very stretched in managing this service and there is a constant conflict between NHS and local Government as to who pays for this service to the extent that in 2035 more money has been spent on Judicial reviews of elderly care in the South West than on the actual provision of care.
Palliative care is reduced to pain management with the 2020s criteria for Do Not Resuscitate stripped back to a Do Not Treat policy which is adhered to in every case admitted to the CDU. Staff burnout in elderly care is high and it is accepted that staff only work in this specialism for a few years. There is therefore little expertise being developed in elderly care interventions and this has become a Cinderella service in terms of R&D.
There is an increasing move towards privatising end of life units as a way to manage demand for care in elderly populations. A confidential paper, drafted after secret discussions between the assisted suicide firm Clementia and the private health insurer BetterHealth facilitated by the UK Government, has been leaked to the press in summer 2035 as a strategy for managing winter pressures in 2036. The paper proposes a strategy for voluntary euthanasia to be available to the over 85s. The BMA ethics committee publicly commented on the leaked paper, saying now was the time to consider all humane options and that the Clementia model of compassion was highly regarded and should be considered as one option to meet the soaring demand in elderly care.
There is an increasing polarisation in the workforce between staff trained before 2020 and newly trained staff. Staff who were trained prior to the acute covid years continue to leave the service disillusioned or suffering from symptoms of moral injury, catalysed by their experience during the pandemic and the persistent retriggering that many experienced in the following years of poorly resourced recovery. Those who stay are characterised by cynicism, persistent resistance to change and apathy. Many talk about their purpose as one of staying to serve their pension; staff who express a purpose in relation to serving patients are now regarded as naive, dismissed as the ‘moral high horse brigade’ or the laughable ‘old guard’. A culture of distrust is embedded in the Service, with Trade Unions and Staff Side interventions a daily feature of management activity, leading to chronic delays in decision making, a rise in safety issues and an ever-present fear of litigation which cripple management resources and stifle innovation.
Newly trained staff have gone through a rigorous new curriculum designed around a minimalist health service with career progression rewarded for efforts in efficiencies and meeting targets for reducing patient usage of services. The NHS Graduate Trainee Scheme has replaced general manager training with management consultants training in a groundbreaking transfer of the much loved service scheme to the private sector.
The big three management consultants have competed for the past 10 years to deliver this lucrative 5-year training programme. The initial contract, awarded to the consultancy firm Prospectum, led to a root and branch reset of expectations for NHS managers which shifted the culture in South West NHS services to that of a business mindset and financial purpose.
This has been built on by subsequent providers and the NHS Grad scheme is now regarded as a world leading business training scheme. (The new contract for 2035-40 has been delayed in response to the expression of interest in running the scheme from two individual global entrepreneurs who have issued a legal challenge to the procurement process based on a proposal to extend the UK training programme to a global health workforce model).
Values Based Recruitment (VBR), an indicator of innovation, and ‘Good to Great’ staffing initiatives in the early 2020s have given way to Skill Based Recruitment (SBR), which focuses on technical and financial skill sets and privileges personality traits based on rational thinking, objectivity and emotional detachment. Congruence, empathy and integrity have been removed from NHS leadership and management frameworks and from NHS Assessment Centre criteria. ‘To be human is to be a machine; to care is to be punished’ was the title of a suicide letter from an NHS Nurse who took her own life following her 6th clinical leadership application rejection. Her letter, sent to the online BMJ on the day of her death, documented years of systematic disinterest from South West NHS leaders and Regional Bodies. Disinterest in relation to the deterioration of care and humanity in the wards at her local hospital where financial efficiency and discharge were the determining factors in care choices, and where the needs of the patient had become, in her experience, a question that incurred managerial reprimand. There was a short-lived news interest in her story but this was overridden by the BBC breaking news event that leaked the hospital’s inclusion on the list for decommissioning hospitals in 2036 on the grounds of bankruptcy.
Integration has also failed to live up to the promises of a decade ago and the energy for transformation has been lost from the culture of system leadership.
The NHS and local government often find themselves in a struggle against one another when it comes to gaining influence and accessing resources. In 2035 we have a new shared purpose for leadership of integration in the South West public sector - resistance. We no longer pretend that integration is desirable and there is an open collusion, a Faustian pact, between different agencies that protecting siloes is important.
The 10-year Plan for Places commissioned by the new Government in 2024 was written in the South West as a shared act of resistance to the imposition of National Government pronunciations on the nuances of South West identity. With National Government preoccupied with post covid recovery and public Inquiries, the 10-year plan was approved without much scrutiny and was mostly a rehash of old and contested differences from previous ICS and STP plans. As such it allowed for ten years of legitimised cross system competition and protection of silos in local systems. The revised plan of 2034 is today the subject of a judicial review, with legal action threatened to South West NHS Boards and the new South West Regional Council for failing to ensure integration of addiction services which have been deemed a Government priority for communities in 2035.
There is a Mental Health Pandemic in the general population following the impact of covid and the failure of successive governments to acknowledge and mitigate this.
The health and social care workforce are one group who have been hit particularly hard as the impact of moral injury from the covid experience and subsequent public inquiries about the role of government in key factors such as PPE and lockdown decisions reveal that more could have been done to prevent the high UK death toll. Key research findings in 2021/22 about the MH impact of covid on health and social care workforce were used as political footballs. This acted as an avoidance of confronting the unbearable reality of a health and social care community breaking down instead of a shared national response to the growing MH crisis. As a consequence, the workforce today is psychologically replete and demoralised. Addiction is high amongst clinicians and safety events are frequent and under monitored because of the volume of incidents. Occupational Psychology teams are overwhelmed and the 2020 focus on compassionate leadership has been replaced with a focus on dispassionate care as a means of staff survival.
Amongst the general public, demand for MH services is unsustainable and US style street scenes, prevalent a decade ago, are now commonplace with mentally ill and uncared for people sleeping rough, drinking on the streets. This huge volume of unmet need has had a knock-on impact on policing and prison services which are frequently overwhelmed in dealing with mental health needs. Volunteer members of the public take on the mantle of care on the streets and at home as formal MH services crumble and are only able to deal with acute illness. Admissions to MH wards have increased, and there is a shift in policy to increase MH beds and reduce community treatments in favour of a community MH policy that is not well enough resourced or trained to cope with the volume and complexity of mild and moderate MH conditions that now dominate UK health profiles.
Homeless shelters and supported accommodation now only accept female residents in a vulnerability-based criteria that has also seen a 60% reduction in occupancy in 2035 compared to 2025. Winter deaths amongst homeless groups have soared since 2025 and annual temporary morgues to deal with winter mortality across the population have become the norm in 2035 - a familiar and accepted community reality since the covid third wave of Winter 2021.
Today, commissioning of services is no longer debated as an indicator of need. At best, today, commissioning of services is a financial exercise to ensure critical services can continue whilst demand is reduced for all other services. At worst it is a managerial and bureaucratic exercise to ensure that accountability for taxpayers’ money is maintained, prioritising staying in credit financially, with little reference to what is actually needed by patients and communities. Our last South West Integrated Care System Board in June 2035 was held as an emergency meeting following the Board’s Summer Report which showed a predicted overspend by £73.4 million in 2035, and the subsequent removal of the CEO and DOF from their roles. The meeting was attended by an NHSE turnaround CEO and interim DOF who gave assurances to the Board that a new regime was being put in place and that providers had been issued with new contracts and budget priorities for service delivery.
In 2019 The King’s Fund identified a large and growing gap between capacity and demand in district nursing services, with staff reporting feeling ‘broken’, ‘exhausted’ and ‘on their knees’. There was a 35 per cent reduction in health visitors in England’s NHS between 2015 and 2020 and a 38 percent decrease in learning disability nursing numbers between September 2010 and September 2019. These figures doubled between 2021 and 2024 with the result that community services were no longer a viable option, and vocational routes for staff became limited to general nursing roles with limited career specialisms and generic, ‘one size fits all’ services to patients.

The role of leadership
In 2035 leaders are recruited, trained and rewarded for stamina, ability to compromise and flexibility with values. The language of burden, crisis, control and efficiency dominate the South West leadership discourse; despite rhetoric to the contrary, managerialism is promoted above leadership and performance is measured by adherence to protocol, procedure and bureaucracy.
Leaders have consequently adopted an increasingly tight managerial approach, based on centralising work priorities and controlling activity as a way to manage change fatigue and unrest in the workforce. The proposed approach to compassionate leadership advocated by national experts at the Queens Fund (where autonomy, belonging and competence are valued) has been replaced by a new proposal in which rule compliance, working in professional units, rather than across teams and systems, and financial competence are most valued.
The unintended consequence of pressure by the central government means that work needs to be done at a higher level where people in leadership roles are more reluctant to change and politics comes into play.
We thought the politics issue should sort itself out when we formally integrated as there would only be one organisation and one board. But it didn't, it got worse.
This comment from the South West staff survey revealed the ongoing and now chronic problem with political maneuvering and organisational competition locally.
Clinical leadership is discouraged and clinical development is limited to medical specialism as needed. There is an emerging culture which views clinicians as an old elite who have been pampered and over invested in as a profession. In 2035 there is a South West approach to investing in managerial and operational leadership as a way to redress this perceived imbalance and to support achievement of performance objectives.
Turnaround leaders have evolved to become the most powerful leadership roles in the country. In the South West, ‘The Taunton Group’ as they have become known, are one of the most powerful Networks in the country and are regularly drafted in to sort failing systems across the UK. The Group is used as the benchmark for leadership attributes which include comfort with difficult conversations, assertiveness, single mindedness; the refusal to compromise and the promotion of public humiliation of managers as a performance motivator.
The Group cut its teeth on a seminal turn around process in Devon in 2029 where two-thirds of the management team in each NHS organisation in the City were removed over a 2-month period. Recruitment giant Hart worked in partnership with NHS Providers and the Turnaround team to source a fully operational, international replacement management team within 6 weeks. Attractive salaries were offered to the new managers for an 18-month contract and when that ended in 2030 staff were let go and services were further centralised under super manager structures of 60 people to one line manager. The savings created by this Turnaround process were significant and a new model of Turnaround was written up by the Group in partnership with Ross Business school who came on board to deliver a ten-year contract for staff development based on this approach.
A new behavioural framework was developed by Ross in 2030, based on the capabilities and behaviors of the Taunton Group. This has been adopted by all NHS organisations as the benchmark for future leaders following a presentation to the Commons Health and Social Care Committee when it convened a special meeting to explore connecting Business agendas and Health agendas at the House of Lords in 2032.
A study exposing bullying, incivility and corporate coercion in the NHS in early 2000’s was reframed in 2030 as constructive form of leadership based on assertive, commanding, and collective leadership. The experience of civil contingency measures during the pandemic highlighted the benefits of command and control leadership, such that collaborative and distributed leadership models became redundant in a culture that is now organised around financial efficiencies and management safety. Combined with the financial success of the Taunton Turnaround Group methods, this framing of leadership dominates assumptions and expectations of what is acceptable for leaders in 2035.
Access to personal development and leadership programmes in the South West is encouraged if recommended by your line manager but there is a three-year backlog of applications waiting for approval at the annual assessment meeting.

Being a patient in the South West in 2035
Josh is 3 and lives in Gloucestershire. Three months ago, after a bout of flu, his Mum suspected that something was amiss. Josh often wet the bed, was constantly thirsty, and was tired and irritable for weeks. Josh’s mum tried to arrange an appointment with the GP but the first emergency appointment was more than two weeks away. Josh’s Mum decided to take Josh straight to A&E. After a six hour wait, Josh was seen and after investigation it was discovered that Josh had suffered from diabetic ketoacidosis (DKA). He remained in hospital for two weeks then was referred to the paediatric diabetes service.
Luckily for Josh and his Mum, the paediatric diabetes services for the South West is located within Gloucestershire so its relatively easy to get to appointments. Other families from Cornwall have to travel many miles across the region to access support. A diabetic nurse talks to Josh’s Mum and explains that training to manage Type 1 diabetes is largely undertaken through group work but there was none planned for the coming 6-8 weeks; that was dependent on staff being available and if a big enough group of people could be brought together in one place. That was difficult to arrange. In the meantime, a diabetic nurse would try to come out to their house to talk to the family but that might take some time. The best thing for now, the nurse explained, is to look online and wait for us to get to you to go through some training.
Josh’s mum feels left on her own to manage and is worried she doesn't have the skills or knowledge to keep Josh well.
Workforce profile
Total workforce size in 2035: 352,000. Overall staffing levels have increased by around a fifth since 2020 across all health and social care services. However, this represents a relative shrinkage given the much larger increase in the elderly population of the South West, causing demand for services to rise rapidly both in terms of complexity and in sheer scale.
Fastest growing health and social care occupation
NHS nurse (35% increase since 2025). Acute, hospital-based services have increasingly been prioritised as the maintain standards within funding realities, with aggressive recruitment drives taking place for extra NHS nurses in response to growing public outrage at growing waiting times for acute care. However, declining investment in preventative treatments and care has had the effect of driving demand for acute services higher still, meaning that there remains considerable reliance on agency and bank staff to complement this increased NHS nursing workforce.
Other key trends
One long-lasting consequence of the Covid-19 pandemic has been a rise in prominence of mental health as a key area of concern for health and social care services: both in terms of the enduring impacts of the lockdowns of 2020-21 on the wellbeing of the population as a whole, and more specifically with regards to the trauma felt by many of the health and social care workers who were at the front-line of the pandemic, which proved difficult for many staff to recover from.
In response to huge public concern regarding this issue, successive governments have put considerable resources towards helping the NHS deal with Britain’s mental health crises, which has mainly been manifested in the South West by a rapid rise in the numbers of mental health nurses. However, most of these additional mental health nurses find their jobs mostly taken up with addressing the symptoms of the mental health crisis, including rising numbers of people experiencing severe depression; across the health and social care system, overworked staff simply do not have sufficient capacity to undertake the kind of preventative action that could help address the root causes of the crisis.

Staff survey results
- 22% of staff are satisfied with their level of pay (down from 38% of NHS staff in 2019.)
- 63% of staff report feeling unwell as a result of work-related stress in the past 12 months (40% in 2019).
- 52% of staff feel that their manager takes a positive interest in their health and wellbeing (70% in 2019).
- 48% often think about leaving their organisation (28% in 2019).
- 15% feel valued for their work.
- 25% believe they experience autonomy, belonging and purpose in their work (the three pillars of effective leadership established as a benchmark by the DH&SC following a report by Michael West in 2025 and still espoused as the system standard in 2035.)

Impact of Brexit on the workforce
The short-term impact of Brexit was to intensify the staffing shortages experienced by services in the immediate post-pandemic period. By the end of 2022, however, the numbers of those leaving the workforce due to fatigue and stress became so large the UK Government instituted new incentives for non-British nationals to come and work for the NHS and in social care.
In particular, a new Immigration Health Payment of £800 was offered to all migrants who took up a position in health and social care within six months of moving to the UK. Moreover, with normal travel to the UK still suspended for the many parts of the world where Covid-19 continued to rage, the UK Foreign Office began running dedicated flights in early 2023 to transport health workers willing to move to the UK from countries including India and Nigeria. Full two-jab vaccination and paid-for hotel quarantining was provided for all migrating health and social care workers from countries where herd immunity from the virus had not yet been achieved.
By the early 2030s, workers from non-EEA countries make up around 15% of the South West’s health and social care workforce - around a doubling in this proportion since 2023. Staff remain so stretched despite this in part because of a long-term, continuing decline in the numbers of EEA migrants willing to come and work in a UK which by now has diverged from the EU quite dramatically with regards to key environmental, social and labour market standards: just 2% of NHS workers in the South West come from EEA countries by 2035 in this scenario, down from 5.5% in 2020.
The role of clinicians
- Clinicians work hard to manage processes to ensure that certain groups are not excluded, by ensuring that the individual patient is kept at the centre.
- We see the emergence of health consumers, bringing new data and potentially privately purchased test data/results into their interactions with doctors. These make for more challenging interaction with patients when doctors haven’t previously seen them.
- There is more emphasis on a shared responsibility/ accountability and diminished, smaller teams making clinical judgements.
- Doctors have self-care deeply built into their training to combat the explosion in mental ill health in the profession.
- Overstretched doctors complain they cannot be expected to know the entire holistic view of an individual patient’s complexity. There remains a strong emphasis on supporting patients through shared decision making.

How we got to 2035
-
General election, a Government is formed.
-
Brexit and the United Kingdom leaves the European Union.
-
COVID-19 pandemic impacts on the life of every citizen. The South West is locked down both socially and economically.
-
As a result of the measures taken to mitigate the risk to human life from COVID-19 recession hits the UK hard and the UK government borrowing reaches 150 percent of GDP.
-
Public services cuts amidst a tightening of budgets due to a recession.
-
Public sector protests across England, driven by those deemed 'critical workers' during the 2020 pandemic lead to a general strike, resulting in the creation of a new Commission on Health and Care.
-
The great Pandemic Public Inquiry.
-
UK Foreign Office begins running dedicated flights to transport health workers willing to move to the UK from countries including India and Nigeria.
-
The Covid Care Act of 2022.
-
General election - the incumbent government loses and opposition parties are invited to form a new Government on a platform to negotiate a new relationship with the EU and introduce a citizens’ income.
-
European Convention on Human Rights re-enshrined in UK law.
-
A renewed focus on Place as the boundary for systems is set out as key manifesto priority and as a new 10 year Plan for Places is commissioned by The Government and set as a priority task for every local System.
-
The NHS Graduate Trainee scheme is offered to the market and is awarded to Prospectum who propose a root and branch reset of NHS workforce expectations. A new curriculum based on business skills and demand management is implemented and NHS jobs enter Business School career development portfolios.
-
Introduction of a Citizens’ Income and Universal Credit is withdrawn.
-
More money has been spent on Judicial reviews of elderly care in the South West than on the actual provision of care.
-
Regional devolution referenda are held and passed by popular vote across England, ultimately turning England into a more federal country. The South West elects its first regional Mayor.
-
Creation of waves of new technical jobs with the growing impact of AI.
-
Regional assemblies created across England, including the South West, with powers devolved to the local level, based strongly on the principle of subsidiarity. Regional elections held. Local activism and community-led citizen participation increases.
-
Voting age for all elections is lowered to age 16.
-
UK joins the European Economic Area (EEA) (on a Norway-plus basis) after four years of intense UK-EU negotiations.
-
General election - a breakthrough number of Independent MPs representing community interests - building on the strength of their local/regional devolution platforms and supported by the newly enfranchised youth - are elected.
-
Suicide Service established
-
Regional assembly elections held.
-
Despite liver disease now being the third largest cause of death in the South West, the development of the 2034 Bristol City Alcohol Plan marks an all-time low in South West integration relationships.
-
General election, a Government is formed